In the autumn of 1927 eight-year-old Murray Fraser caught a bad cold. He was lethargic, had a sore throat, a mild fever, and chills. But this was no ordinary cold. Soon he felt sicker than he had ever felt in his life. His mother summoned the doctor, who determined that a throat swab was warranted. It would take a few days for a Winnipeg lab to confirm a diagnosis.
Annie Fraser was having none of it, and insisted her boy be given an antitoxin immediately. She was right. It was diphtheria, and the quick action probably saved his life.
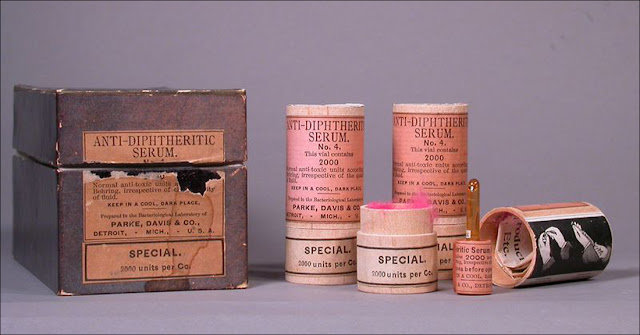 |
| Early samples of antitoxin serum for diphtheria [Warner, 2013] |
Known to the Greeks in the 4th century B.C., diphtheria is not a new disease. During a 17th century epidemic, the Spanish termed it “The Strangler,” and it appeared in New England in the early 1700s. By 1900 it was one of the leading causes of death for infants and children.
Extremely contagious, diphtheria is airborne, typically spread through person-to-person contact, coughing and sneezing. With a two- to five-day incubation period, it is one of the fastest moving diseases, and its victims die quickly, either from suffocation or the spread of toxin in the bloodstream that can cause heart failure or paralysis. [Ciok, 2000]
The Centre for Disease Control (CDC) describes how frightful and horrid diphtheria is:
Early symptoms include malaise, sore throat, anorexia, and low-grade fever (less than 101°F). Within 2 to 3 days, a bluish-white membrane forms and extends, varying in size from covering a small patch on the tonsils to covering most of the soft palate. Often by the time a physician is contacted the membrane is greyish-green or, if bleeding has occurred, black. [...] The membrane is firmly adherent to the tissue, and forcible attempts to remove it cause bleeding. Extensive membrane formation may result in respiratory obstruction.
While some patients may recover at this point without treatment, others may develop severe disease. The patient may appear quite toxic, but the fever is usually not high. Patients with severe disease may develop [...] a characteristic “bull neck” appearance. If enough toxin is absorbed, the patient can develop severe prostration, pallor, rapid pulse, stupor, and coma. Death can occur within 6 to 10 days.
Without an antitoxin, doctors could offer few remedies beyond tracheotomies and intubation to counteract the suffocation. Diphtheria kills 5–10% of sufferers, and up to 20% of those under age five or older than 40. In the U.S. in the 1920s there were between 100,000 and 200,000 cases each year, with 13,000–15,000 deaths. [IAC, n.d.]
In 1924, the worst year for diphtheria in this country [Canada], there were 9,000 cases and 2,000 deaths.
A diphtheria antitoxin had existed since 1894. It was produced in many countries but not in Canada, where it had to be imported from the U.S. at a price so high that one in every three children infected with the disease died.
What Canada needed was a public health laboratory capable of producing and distributing diphtheria antitoxin in the quantities needed, at a price that would be affordable for all. In 1913 this challenge was taken up in Toronto by 31-year-old John Gerald FitzGerald. Driven by his determination, a diphtheria antitoxin would eventually be free and the foundations of vaccine research, development and production would be built in Canada, with consequences that would be felt worldwide. [Longley, 2020]
 |
| FitzGerald’s Connaught Antitoxin Laboratory at the University of Toronto was an industry leader. [Rutty, n.d.] |
In Canada, campaigns to inform the public and encourage vaccination were numerous. Efforts included short health films to educate moviegoers about the need to get vaccinated against diphtheria and smallpox. A February 16, 1927 article in the Lethbridge Herald explained that “The view commonly held that vaccine is a filthy material taken from the ulcerated sore of a diseased cow was disproved.” The old-time sulphur and molasses treatment for illness would only spread an epidemic.
 |
| The Lethbridge Medical Society produced two health films shown with the regular offerings in its movie theatres. [Lethbridge Herald, February 16, 1927, p. 10, emphasis added] |
In a 1955 Maclean’s magazine article, June Callwood explained how the diphtheria antitoxin was produced:
Diphtheria is caused by bacteria that settle in the throat and pour out poison, or toxin. To produce diphtheria antitoxin, this poison is injected in minute quantity into the bloodstream of a horse, causing the horse’s body to form substances—known as antibodies—to fight off the invading poison. The next injection contains more toxin, which produces more antibodies in the horse’s blood. Eventually, after about four months of injections, the horse can tolerate without discomfort an injection strong enough to kill a thousand horses; his blood is hyper-immunized. This blood, drawn off in small quantities at regular intervals, is treated to become diphtheria antitoxin. When it is injected into a human suffering from diphtheria it bolsters the victim’s feebly developing antibodies and results in a cure. Antitoxin is used in the treatment of diphtheria; diphtheria toxoid, developed in 1924, is used to prevent the disease. [Callwood, 1955]
If young Murray Fraser had known the contribution horses had made, perhaps he would have had a better opinion of them. Recent efforts are exploring ways to make diphtheria treatment without injecting horses with toxin. [Kupferschmidt, 2020]
Murray was fortunate to have recovered unscathed. His four-year-old cousin Mildred Fraser was not so lucky.
 |
| Murray Fraser with his cousin Mildred and his sister Jessie |
 |
| Carman Dufferin Leader, October 27, 1927 |
The disease was raging in the area, but Murray always worried that his cousin had caught the disease from him. The newspaper hints at this: “Mr. and Mrs. Fraser were visiting here up until a week ago, and it was immediately after their return home to Carman that news was received here of their loss.”
In Canada during the 1920s diphtheria remained a leading cause of death for children under 14, despite the availability of diphtheria antitoxin. Dr. John G. FitzGerald, founder of Connaught Laboratories in Toronto, led the world’s public health war against diphtheria, conducting Canadian field trials between 1926 and 1931, and producing a new toxoid on a large scale. [Rutty, 1996]
The challenge was to get the vaccine into the arms of susceptible children.
 |
| Another four-year old dies of diphtheria. Pilot Mound Sentinel, November 17, 1927 |
The two deaths prompted action. The same newspaper that told of the death of the Laird boy announced a ban on all public gatherings:
 |
| Front page notice in the Pilot Mound Sentinel, November 17, 1927 |
The ban remained in effect a week later:
 |
| Pilot Mound Sentinel, November 24, 1927 |
Impressive public health efforts battled diphtheria and numbers dropped as vaccinations became commonplace. Health officials in Brandon, for instance, launched extensive campaigns to encourage immunization, and results were encouraging. Manitoba editors pushed for aggressive efforts:
It is a well established fact that smallpox, diphtheria and typhoid fear can be absolutely prevented and banished from our midst. These frightful diseases can be rendered extinct as the dodo, leprosy or yellow fever. Yet they continue to stalk through the land claiming their thousands of victims every year. Why? Because of what amounts to criminal negligence on the part of health officials and people generally.
Our Western prairie provinces pride themselves in their work for the promotion of health, but they still have a long way to travel in the direction of the eradication of preventable disease. There is much educational work yet to be done, and it is sincerely to be hoped that provincial health departments, municipal councils and health offices, all doctors, and every organization interested in the health, happiness and well-being of the people will throw themselves unreservedly into the campaigns now in progress [...] for the wiping out of preventable disease. The community which does not engage in this warfare stamps itself as hopelessly backward, and indifferent to the best interests and highest welfare of its people. [Baldur Gazette, April 7, 1927]
A Creston Review editorial claimed that many illnesses were largely preventable, and warned that preventable death breaks up the home and can lead to juvenile delinquency. That would lead to poverty, improper living conditions and a breeding ground for disease, creating a vicious cycle. An extreme argument, perhaps, but the editorial ended on a wise note: “Science has made possible the accomplishment of this highly desirable result. It remains for the people to inform themselves and profit by the information which is so readily available to them.”
That last point rings true today.
Canada has one of the lowest child vaccination rates in the developed world. With about one-tenth of Canadian children now going unvaccinated, this means that up to 750,000 young Canadians have no immunity whatsoever against diphtheria, whooping cough, tetanus and measles. [… Federal Government efforts need to remind] Canadians of the alternative to vaccination: A country wracked by fear, tragedy and landscapes of dead and paralyzed children.
As late as the 1920s diphtheria was killing up to 2,000 young Canadians every year. Even as late as 1943, vaccination apathy meant that the disease was still able to kill 200. Diphtheria hasn’t killed anyone in Canada since 2000, but the disease remains in check purely due to immunization. [Hopper, 2019]
 |
| Number of cases of diphtheria in Canada [Government of Canada, 2018] |
The arrow marks 1926, the year in which Canada introduced the diphtheria vaccine. Cases start at 9057 in 1924. Between 1929 and 1931 a sharp decline from 9010 to 2031 cases is shown. Another decline begins in 1945 and cases are down to 38 by 1959. From 1984 onward fewer than 10 cases were reported each year, and between 0 and 4 cases were reported between 1992 and 2012. [Government of Canada, 2018]
Today, Canadians give little thought to diphtheria because it is prevented by routine vaccination. But some may recall it through heroic Arctic tales from the 1920s.
In the winter of 1925, a dogsled relay rushed diphtheria antitoxin from Anchorage to Nome, Alaska in what became known as “The Great Race of Mercy.” In temperatures nearing –50˚F several teams took a mere 5½ days to make the dangerous 674-mile (1085 km) trek.
Four years later in similar winter conditions, pilots Wilfred “Wop” May and Vic Horner made history by flying diphtheria serum 410 miles (660 km) from Edmonton to Fort Vermillion in an open cockpit Avro Avian. (May was already a notable World War I pilot. His was the plane the Red Baron was chasing when the Baron was finally shot down.)
May’s story was featured in a National Film Board vignette:
Although we no longer fear it, diphtheria has not been eradicated world-wide. We would all be wise to heed the lesson Annie Fraser and her family learned. Listen to the science and don’t be complacent.
Do it for Mildred.
 |
| Murray Fraser and his wee cousin Mildred, in front of Gordon Fraser’s harness racing truck. |
Sources
“About Diphtheria,” Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/diphtheria/about/index.html, Retrieved July 9, 2021
June Callwood, “The Miracle Factory that began in a Stable,” Maclean’s. October 1, 1955. https://archive.macleans.ca/article/19551001017/print Retrieved July 9, 2021
Amy E. Ciok, “Horses and the Diphtheria Antitoxin.” Academic Medicine. Vol. 75, Issue 4, 2000. https://journals.lww.com/academicmedicine/fulltext/2000/04000/horses_and_the_diphtheria_antitoxin.22.aspx Retrieved July 9, 2021
“Diphtheria Causes Death of Little Boy,” Pilot Mound Sentinel, November 17, 1927
“Diphtheria: Questions and Answers,” Immunization Action Coalition (IAC), n.d. https://www.immunize.org/catg.d/p4203.pdf Retrieved July 9, 2021
Government of Canada, “Diphtheria for Health Professionals,” Ottawa, April 17, 2018 https://www.canada.ca/en/public-health/services/immunization/vaccine-preventable-diseases/diphtheria/health-professionals.html#fig1 Retrieved July 9, 2021
Tristan Hopper, “Vignettes from a pre-immunization Canada as childhood vaccination rates plummet.” National Post. June 26, 2019. https://nationalpost.com/news/canada/paralysis-spreads-throughout-canada-horrific-reminders-from-a-pre-vaccination-age Retrieved July 9, 2021
Kai Kupferschmidt, “Scientists find way to make diphtheria treatment without injecting horses with toxin.” Science, January 17, 2020. https://www.sciencemag.org/news/2020/01/scientists-find-way-make-diphtheria-treatment-without-injecting-horses-toxin Retrieved July 9, 2021
Richard Longley, “Toronto pandemics past: Diphtheria ‘the strangler’ “ NOW Magazine, April 26, 2020. https://nowtoronto.com/news/toronto-pandemics-past-diphtheria-the-strangler Retrieved July 9, 2021
“Promoting Health—Preventing Disease,” Creston Review editorial, December 2, 1927
“Puts Ban on All Public Gatherings,” Pilot Mound Sentinel, November 17, 1927
Christopher J. Rutty, “Connaught and the Defeat of Diphtheria.” Conntact (Connaught Employee News), Vol. 9, No. 1, February 1996. http://www.healthheritageresearch.com/Diphtheria-conn9602.html Retrieved July 9, 2021
Christopher Rutty, “History of Connaught.” Defining Moments Canada, n.d. https://definingmomentscanada.ca/insulin100/timeline/connaught Retrieved July 9, 2021
“Sad Death of Little Fraser Girl,” Pilot Mound Sentinel, November 3, 1927
“Show Health Films,” Lethbridge Herald, February 16, 1927
“Too Late!” Baldur Gazette editorial, April 7, 1927
Mallory Warner, “How horses helped cure diphtheria.” National Museum of American History, August 15, 2013. https://americanhistory.si.edu/blog/2013/08/how-horses-helped-cure-diphtheria.html Retrieved July 9, 2021

